Every now and then, we get a phone call from a patient who we saw a couple of days earlier. It goes something like this:
I had a filling done on my last tooth on the lower left three days ago. The filling and tooth feel fine, but it hurts to open my mouth, especially if I try to open wide.
We then go on to explain to our patient WHY this is the case and how it is normal.
So why is there pain with opening? There are two major factors.
Dental Injections for Lower Molars
In many cases, the pain while opening is from the injection. For lower molars, most dentists will do a nerve block, which involves a very long needle. See the photo below.

A dental injection used to anesthetize a lower right molar. The needle in this photo is 1 and 1/4 inches long.
As can be seen in the above photo, a needle is inserted into the muscle in the back of the mouth. In most cases, for this injection, the needle goes in nearly to the hub, which would mean approximately 1 and 1/4 inches.
Here’s an analogy: feel your biceps and press it hard enough so you can feel the bone underneath. Then, imagine taking a needle, and inserting it through the biceps, approximately 1 inch, until the needle hits bone. Then, imagine doing that a second time. Don’t you think that moving the arm and using that muscle over the next several days would hurt?
The biceps analogy is very effective. Everyone understands that their arm would be sore. So, if you get an injection back there, or in some cases two, using that muscle in opening and closing can frequently result in pain for several days afterwards.
Your TMJ (Temporomandibular Joint)
The second source of pain while opening after a filling can be from the actual jaw joint, known as the TMJ (temporomandibular joint). This is the area at which your lower jaw bone connects to the base of the skull.
Your jaw joint was made for all of your daily activities – talking, smiling, eating normal foods, etc. The joint was not designed for “abnormal” tasks such as gum chewing, chewing on ice, or holding your mouth open for your dentist or hygienist to work.
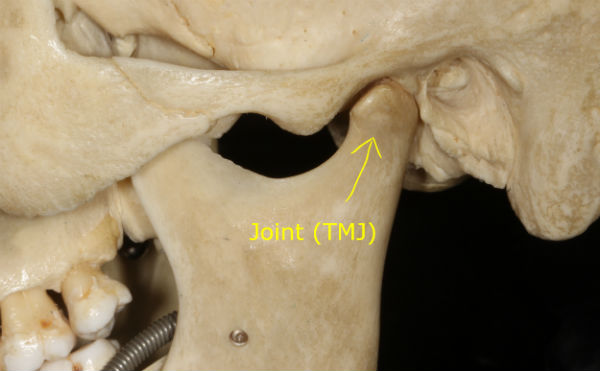
The temporomandibular (TMJ) joint. Pain in this joint as well as the muscles and ligaments associated with the joint can occur after a dental visit.
Here’s another analogy: imagine standing on the tips of your toes. Now do this for 5 minute intervals several times, with perhaps 30 second breaks in between. Do this for approximately 45 minutes. Don’t you think that the next day, moving that muscle and the joints would be sore? This assumes you are not a ballet dancer.
A cleaning or a filling of moderate duration will be a lot like the above. Lots of straining to keep your mouth open, which can lead to fatigue and soreness in the muscles and joint. This can then result in pain and soreness on opening for several days.
Some Assumptions
We find that one or both of these reasons are responsible for the pain and soreness approximately 99% of the time. There are other circumstances which can include:
- Infection of either a tooth or an infection at the injection site.
- Pain after a surgical procedure such as a lower wisdom tooth extraction.
- Aphthous ulcers (cold sores) in the back of the throat.
- Upper respiratory infections, etc.
- And many others.
Of course there can be other explanations. But for the vast majority of the time, the pain is either from the actual injection or in joint after being open for a prolonged period of time.










